Contents
Traditional healthcare delivery often creates barriers such as long travel times, scheduling conflicts, and limited access to specialists. These challenges have accelerated the demand for telehealth website development, allowing healthcare providers to deliver virtual care that is more accessible, efficient, and patient-centric.
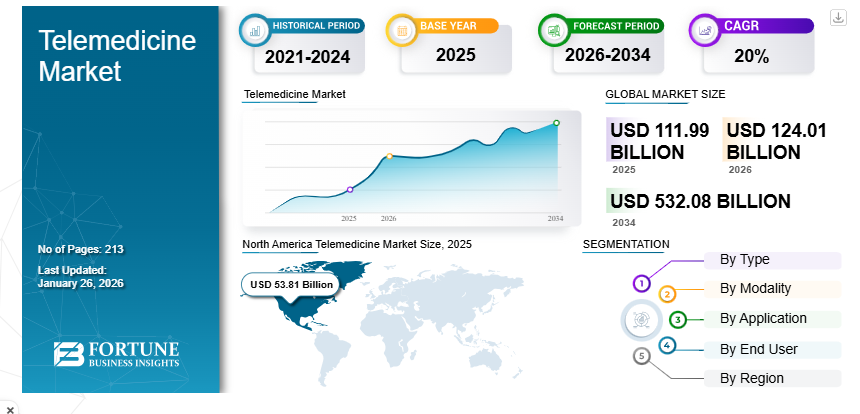
According to the Fortune Business Insights, The global telehealth market, valued at approximately $111.99 billion in 2025, is expected to exceed $532.08 billion by 2030.
For healthcare organizations, investing in telehealth platforms is no longer optional — it is essential for improving patient engagement and staying competitive.
Drawing from Monocubed’s experience in building secure and scalable healthcare web solutions, this guide covers everything you need to know about telehealth website development, including essential features, compliance requirements, technology stack selection, cost considerations, and best practices for choosing the right development partner.
Whether you are a healthcare provider, startup founder, or technology leader, this guide will help you make informed decisions about building a successful telehealth platform.
What is Telehealth Website Development?
Telehealth website development is the process of designing, building, and deploying a web-based platform that enables healthcare providers to deliver clinical services, communicate with patients, and manage care workflows remotely.
It encompasses everything from the patient-facing interface to the provider dashboard, backend integrations, and the security infrastructure that keeps protected health information safe.
Before diving deeper, it helps to clarify the terminology, since several related terms are often used interchangeably but mean different things from a development perspective.
- A telehealth website is a browser-based platform that supports virtual consultations, appointment scheduling, messaging, and billing without requiring patients to install an app.
- A telemedicine app, by contrast, is a native mobile application optimized for clinical consultations on iOS or Android.
- A patient portal is focused on information access, allowing patients to view health records, lab results, and billing history. Here, patient portal development provides you web portal solutions to deliver to cater your patient needs.
- A telehealth system is the broadest term, encompassing all of these components along with provider dashboards, admin tools, and backend infrastructure.
These are different types of web portals designed for healthcare organizations.
This distinction matters because it directly affects scope, budget, and timeline. A healthcare organization that needs a full telehealth system is undertaking a fundamentally different project than one that simply needs a patient portal upgrade.
With the core concept established, the next step is understanding why healthcare providers across the spectrum are making telehealth a strategic investment, not just a pandemic response.
Why Healthcare Providers Are Investing in Telehealth Websites
The decision to invest in telehealth website development is not driven by a single factor. It is the convergence of patient expectations, operational economics, regulatory support, and competitive pressure. Each of these forces independently justifies the investment. Together, they make it unavoidable.
1. Improved patient accessibility
Over 80 million Americans live in Health Professional Shortage Areas, according to the Health Resources and Services Administration (HRSA).
For these populations, a telehealth website is not a convenience. It is the difference between receiving care and going without. Telehealth eliminates geographic, mobility, and scheduling barriers, allowing patients to consult specialists regardless of distance and attend follow-ups without leaving home.
2. Reduced operational costs
Every in-person visit carries overhead: facility costs, front-desk staffing, check-in processing, and waiting room maintenance. For organizations managing thousands of appointments monthly, those savings compound into significant budget impact.
3. Better patient engagement and retention
Virtual visit convenience improves treatment adherence, follow-up compliance, and overall patient satisfaction. Telehealth platforms also enable continuous engagement between visits through secure messaging, health education content, and appointment reminders.
In competitive healthcare markets, patient retention is a direct revenue driver, and telehealth platforms are proving to be among the most effective retention tools available.
4. Expanded care reach and remote monitoring
Telehealth enables specialty practices to serve national patient bases without building new physical locations. When combined with Remote Patient Monitoring (RPM) integration, connecting platforms with wearable devices and home health monitors, telehealth transforms episodic care into continuous monitoring.
This is especially valuable for chronic disease management, post-surgical care, and elderly care, where reducing hospital readmissions directly impacts outcomes and costs.
5. Regulatory and digital healthcare trends
CMS has made expanded telehealth reimbursement permanent. Private insurers have followed. State licensure compacts now enable cross-state practice, and value-based care models reward outcomes over visit volume, making virtual care a natural fit.
Organizations that build these capabilities now position themselves for long-term competitive advantage. Those that delay face increasingly expensive catch-up efforts.
Understanding why telehealth matters sets the foundation. The next question is what specific capabilities a telehealth platform must include to deliver clinical value and meet user expectations.
9 Key Features of a Telehealth Website You Must Include
The features built into a telehealth website determine its clinical utility, patient adoption, and operational value. Below are the essential capabilities that every telehealth platform needs, organized by function.
1. Patient registration and profile management
Registration is the entry point to the platform. It must be simple enough that patients complete it without assistance, yet thorough enough to capture demographics, insurance information, medical history, and consent forms.
Profile management allows patients to update information, view visit history, and manage family member accounts. From a compliance perspective, registration must include identity verification and consent management that satisfies HIPAA requirements.
2. Online appointment scheduling
Patients should be able to view provider availability, select appointment types (video, phone, or messaging), choose time slots, and receive confirmation within minutes. The scheduling system must integrate with provider calendars, handle time zones, send automated reminders, and manage cancellations. For multi-provider practices, intelligent matching by specialty, language, and availability reduces wait times and improves first-visit resolution rates.
3. Secure video consultation
Video is the clinical core of any telehealth platform. The system must deliver reliable, high-quality audio and video with low latency, even on slower connections, while meeting encryption requirements. Key capabilities include one-on-one and group sessions, screen sharing for reviewing results, virtual waiting rooms, and adaptive bitrate streaming that adjusts quality based on bandwidth.
4. Real-time messaging and chat
Not every clinical interaction requires a video call. Secure, end-to-end encrypted messaging allows asynchronous communication for follow-up questions, medication clarification, and care coordination. For high-volume organizations, AI-assisted triage that routes messages to the appropriate provider can significantly improve response times while reducing administrative burden.
5. EHR/EMR integration
A telehealth website that operates in isolation from the provider’s EHR creates duplicate records, manual data entry, and clinical risk. Bidirectional integration with systems like Epic, Cerner, or Allscripts using HL7 FHIR standards allows the platform to pull patient history into consultations and push documentation back automatically. This integration is technically complex but essential for clinical workflow integrity.
6. ePrescription and pharmacy integration
Electronic prescription transmission through networks like Surescripts, including drug interaction checking, formulary verification, and EPCS compliance for controlled substances, allows providers to complete the care cycle within a single virtual visit. Without ePrescription, virtual visits create additional steps that reduce patient satisfaction and clinical efficiency.
7. Payment gateway and billing management
The billing system should support multiple payment methods, real-time insurance eligibility checks, CPT code management for telehealth-specific billing codes, and PCI DSS-compliant payment processing. Integration with practice management or revenue cycle management systems ensures that virtual visits contribute to financial reporting just like in-person encounters.
8. Remote patient monitoring integration
RPM integration connects the platform with blood pressure monitors, glucose meters, pulse oximeters, and wearable devices. Alert thresholds notify providers when readings fall outside normal ranges, while trend visualization supports longitudinal tracking. For chronic disease management programs, RPM transforms the telehealth platform from a consultation tool into a comprehensive care management system.
9. Analytics and reporting dashboard
Real-time insights into appointment volumes, wait times, no-show rates, satisfaction scores, and revenue metrics enable data-driven decision-making. Audit logs and access reports support regulatory compliance. The analytics system should support custom reporting and integration with business intelligence tools.
Turn Your Telehealth Idea into a Fully Compliant, Patient-Ready Platform
From video consultation infrastructure to EHR integrations and HIPAA-compliant architecture, Monocubed helps healthcare organizations design and develop telehealth platforms that deliver seamless virtual care experiences.
With the feature landscape mapped out, the critical question becomes how to build these capabilities while maintaining regulatory compliance, which is the single most consequential aspect of healthcare development.
5 Compliance Requirements to Consider During Telehealth Website Development
Compliance is not a checkbox in telehealth development. It is a property of the entire system that influences every architectural, development, and operational decision.
Non-compliance carries severe consequences: HIPAA fines can reach $1.5 million per violation category per year, and a data breach triggers OCR investigations, class-action lawsuits, and reputational damage that can take years to recover from.
1. HIPAA compliance
The Health Insurance Portability and Accountability Act is the foundational framework for any U.S. telehealth platform handling Protected Health Information (PHI). The Privacy Rule governs how PHI can be used and disclosed. The Security Rule mandates administrative, physical, and technical safeguards for electronic PHI. The Breach Notification Rule requires disclosure within 60 days for breaches affecting 500 or more individuals.
Critically, Business Associate Agreements (BAAs) must be executed with every third-party service that handles ePHI. A telehealth platform using AWS for hosting, Twilio for video, and Stripe for payments needs BAAs with all three. Missing a single BAA creates a compliance gap that can result in significant penalties.
Building a HIPAA-compliant website requires specialized expertise and regulatory knowledge that experienced healthcare development providers like Monocubed deliver.
2. GDPR and global data protection
Platforms serving international patients must also comply with GDPR (for EU patients), PIPEDA (Canada), LGPD (Brazil), and state-level laws like California’s CCPA/CPRA. GDPR is particularly demanding, requiring explicit consent, Data Protection Impact Assessments, and data subject rights including erasure, portability, and restriction of processing. The safest approach is building to the most stringent applicable standard, which then satisfies less restrictive regulations automatically.
3. Data encryption and secure authentication
All PHI must be encrypted at rest (AES-256) and in transit (TLS 1.2+). Multi-factor authentication should be mandatory for providers and administrators, with support for biometrics, TOTP, and hardware security keys. Session management must include automatic timeouts, concurrent session limits, and secure token handling.
For a deeper dive into these practices, our guide on web security best practices covers the technical implementation in detail.
4. Video and communication security
WebRTC provides built-in encryption via SRTP and DTLS. However, if the platform routes streams through media servers for recording or multi-party calls, those servers must be HIPAA-compliant and BAA-covered. Messaging systems require end-to-end encryption for content, metadata, and file attachments, with tamper-proof audit trails.
5. Patient data privacy best practices
Beyond regulatory minimums, telehealth platforms should implement data minimization (collect only what is clinically necessary), role-based access control (billing staff should not access clinical notes), tamper-proof audit logging retained for six years, de-identification for analytics, and granular patient consent management with revocation capability.
Compliance shapes every technical choice. With that understanding in place, the next decision is which technologies to use for building a platform that meets these requirements at scale.
How Much Does it Cost to Develop a Telehealth Website?
On average, healthcare organizations can expect to invest between $80,000 and $200,000 for a fully functional, mid-level telehealth platform — with simpler MVP versions costing less and enterprise-grade systems costing more.
Development costs vary significantly based on scope, complexity, and the development approach. Understanding the cost drivers helps you budget accurately and make informed trade-off decisions.
Telehealth website development cost breakdown
| Platform Type | Estimated Cost | Average Price |
|---|---|---|
| Basic MVP (video, scheduling, patient profiles, payments) | $40,000 – $80,000 | ~$60,000 |
| Mid-Range Platform (EHR integration, ePrescription, secure messaging) | $80,000 – $200,000 | ~$140,000 |
| Enterprise Platform (multi-specialty, RPM, AI, full integrations) | $200,000 – $500,000+ | ~$300,000+ |
| White-Label Customization | $20,000 – $60,000 | ~$40,000 |
📊 Average pricing gives you a realistic benchmark — most healthcare providers investing in a robust telehealth solution fall in the $80,000–$200,000 range, with costs rising as integrations, analytics, and advanced features are added.
3 Key cost drivers in telehealth site development
1. Feature complexity: Telehealth platforms with advanced capabilities such as AI-assisted triage, RPM dashboards, or multi-provider workflows require more engineering effort, increasing both cost and delivery time.
2. Integration requirements: Integrating with EHR systems, pharmacy networks, labs, and billing systems is resource-intensive. EHR integration alone can represent 15–25% of total development cost due to interoperability standards and testing.
3. Compliance and security implementation: Ensuring HIPAA, GDPR, and other regulatory requirements are built into your architecture from day one is significantly less expensive than retrofitting compliance into an existing platform later. Early compliance planning reduces technical debt and regulatory risk.
4 strategies to optimize the telehealth website development cost
- Start with an MVP: Focus on essential telehealth features first and expand based on real usage insights.
- Leverage proven third-party services: Integrate tools for video conferencing, messaging, and payments instead of building them from scratch.
- Adopt modular architecture: Break your platform into service modules so features can be scaled or replaced individually.
- Prioritize differentiators: Invest custom effort where it delivers competitive advantage (e.g., advanced analytics, clinical workflows).
For a detailed breakdown of a healthcare website development cost , we’ve written a dedicated cost guide covering pricing across different project types.
3 Timeline factors that affect the overall development cost
Beyond technical scope, several operational elements influence development timelines and website development costs:
- Stakeholder decision speed: Delays in approvals and feedback loops extend project timelines.
- EHR vendor certification: External certification and interoperability testing can add weeks independent of development work.
- Healthcare domain expertise: Teams familiar with healthcare regulations and clinical workflows deliver faster and with fewer revisions than teams learning healthcare on the go.
Cost and timeline clarity helps secure internal buy-in. But before finalizing your approach, there is a fundamental strategic decision to make: build custom, go white-label, or use a SaaS platform.
Get a Clear Telehealth Development Cost Estimate
Monocubed helps healthcare organizations plan secure, compliant, and scalable telehealth platforms with transparent cost breakdowns, architecture recommendations, and feature prioritization strategies.
Build vs Buy: Choosing the Right Telehealth Development Approach
This decision affects cost, timeline, competitive positioning, and long-term platform control. Each approach suits different organizational contexts.
Telehealth development approach comparison
| Factor | Custom Development | White-Label Solution | SaaS Platform |
|---|---|---|---|
| Upfront Cost | $80K – $500K+ | $20K – $60K | $0 – $5K |
| Customization Flexibility | Unlimited | Moderate | Minimal |
| Intellectual Property Ownership | Full Ownership | Vendor-Owned | Vendor-Owned |
| Time to Launch | 3 – 14 months | 1 – 3 months | Days to Weeks |
| Scalability | Fully Customizable | Vendor-Dependent | Vendor-Dependent |
| Integration Flexibility | Full Control | Limited | Very Limited |
| Long-Term Cost (5 Years) | Lower (No Licensing Fees) | Higher (Recurring Licensing) | Moderate |
| Best Fit For | Startups, enterprises, complex clinical workflows | Mid-size healthcare providers needing faster launch | Solo practitioners and small practices |
1. Custom telehealth web development
Custom development is the preferred approach for organizations that require advanced functionality, deep system integration, or strong competitive differentiation. It allows healthcare providers to build telehealth platforms tailored to unique clinical workflows, patient engagement models, and regulatory requirements.
Custom platforms provide complete intellectual property ownership, enabling organizations to control platform evolution, scalability, and feature innovation. This approach is especially valuable for:
- Health-tech startups building telehealth as a core product offering
- Large healthcare networks requiring multi-specialty workflow customization
- Providers needing advanced EHR interoperability and integration flexibility
- Organizations prioritizing long-term scalability and differentiation
2. White-label telehealth solutions
White-label telehealth platforms allow healthcare organizations to launch virtual care services quickly using pre-built infrastructure that can be partially customized. This approach reduces development time and upfront investment while providing essential telehealth capabilities.
White-label solutions are well suited for mid-size healthcare providers that require faster time-to-market and standard telehealth workflows. However, organizations must consider potential limitations, including restricted customization options, vendor dependency, and cumulative licensing fees that may increase total ownership cost over time.
3. SaaS-based telehealth platforms
SaaS telehealth platforms provide ready-to-use virtual care functionality with minimal setup and investment. These platforms typically include standard video consultation features, appointment scheduling, and basic patient management tools.
SaaS solutions are ideal for solo practitioners and small healthcare practices seeking quick telehealth adoption without development overhead. However, they often lack customization flexibility, advanced integration capabilities, and differentiation opportunities required by growing healthcare organizations or digital health startups.
While custom healthcare development involves higher upfront investment, it typically results in lower long-term costs due to the absence of recurring licensing fees and vendor restrictions.
The website development approach determines what you can build. But equally important is who builds it. Here, choosing one of the website development partners directly impacts clinical quality, compliance risk, and platform viability.
How to Choose the Right Telehealth Website Development Company
Selecting a website development partner for a telehealth platform is a decision with clinical, regulatory, and business implications. Evaluate candidates against five criteria that matter most in healthcare development.
1. Healthcare domain expertise
Healthcare domain knowledge separates experienced development partners from general software vendors. A team familiar with clinical workflows, provider-patient interactions, and healthcare operational challenges can design platforms that align with real-world clinical needs.
When evaluating a partner, ask:
- Which healthcare domains have they built solutions for?
- How do they design clinical workflows and user experiences?
- Do they have team members with healthcare industry experience?
Partners with proven healthcare experience can anticipate compliance requirements, design clinician-friendly workflows, and reduce costly redesigns during development.
2. Demonstrated compliance and security experience
Healthcare compliance is non-negotiable. A qualified development partner should demonstrate practical experience implementing HIPAA and other regulatory requirements rather than simply claiming compliance expertise.
Key areas to verify include:
- Data encryption and secure storage practices
- Audit logging and monitoring capabilities
- Role-based access control implementation
- Business Associate Agreement (BAA) management
- Experience supporting certifications such as HITRUST or SOC 2
Strong compliance implementation reduces regulatory risks and ensures long-term platform sustainability.
3. Integration and interoperability capabilities
Telehealth platforms must seamlessly integrate with EHR systems, pharmacy networks, billing platforms, and third-party healthcare services. Integration complexity significantly affects both development timelines and overall project cost.
Evaluate whether the development partner has experience with:
- Major EHR systems such as Epic, Cerner, and Allscripts
- Healthcare data standards including HL7 FHIR and HL7 v2
- Integration engines and interoperability frameworks
- Pre-built connectors that accelerate EHR integration
Partners with established integration experience can significantly reduce implementation complexity and deployment time.
4. Portfolio quality and proven healthcare results
A reliable telehealth development partner should demonstrate real-world success through live healthcare platforms rather than conceptual presentations. Reviewing actual project outcomes helps assess technical quality, user experience, and clinical workflow effectiveness.
When reviewing portfolios:
- Request references from healthcare clients
- Evaluate user interface and patient usability
- Assess workflow alignment with clinical processes
- Review platform scalability and performance
Examining delivered healthcare solutions provides insight into the partner’s ability to handle complex regulatory and operational requirements. Reviewing platforms developed by experienced healthcare technology providers, such as those delivered by Monocubed, can help benchmark expected quality and performance standards.
5. Post-launch support and long-term scalability
Telehealth platforms require continuous updates to maintain regulatory compliance, security standards, and evolving clinical needs. Development should not end at deployment.
Assess the partner’s ongoing support capabilities, including:
- Managed maintenance and compliance updates
- Security patch management
- Performance monitoring and optimization
- Response time for critical technical issues
- Ability to scale development resources as platform usage grows
A strong post-launch support model ensures long-term platform stability and compliance readiness.
Choosing the right development partner ensures your telehealth platform meets clinical, regulatory, and business requirements from the start.
With the right partner and development approach in place, healthcare organizations must also consider future industry trends because telehealth platforms built today must be designed to support tomorrow’s digital healthcare innovations.
Partner with Experts Who Have Built Real Telehealth Platforms
From MedCall to TelaSight, Monocubed has delivered innovative healthcare solutions backed by 200+ successful projects and a 98% client satisfaction rate. We help healthcare organizations build scalable, compliant, and future-ready telehealth ecosystems.
5 Future Trends in Telehealth Website Development
Telehealth is advancing at a rapid pace, and platforms built today must be designed with flexibility to support innovations that are expected to become industry standards within the next three to five years.
Healthcare organizations investing in telehealth website development should anticipate these emerging trends to remain competitive, compliant, and clinically effective.
1. AI-powered remote care and clinical decision support
Artificial intelligence is shifting from an experimental add-on to a core component of virtual healthcare delivery. Modern telehealth platforms are beginning to integrate AI-driven clinical decision support tools that assist providers during virtual consultations by suggesting potential diagnoses, identifying care gaps, and flagging possible drug interactions.
Additionally, Natural Language Processing (NLP) is transforming clinical documentation. AI-powered transcription tools can automatically generate structured visit notes from virtual consultations, reducing administrative workload and helping healthcare providers spend more time focusing on patient care. As physician burnout remains a growing industry concern, automation-driven documentation will become a critical differentiator for telehealth platforms.
2. Hybrid care models becoming the standard
The future of healthcare delivery is not purely virtual or in-person—it is hybrid. Patients increasingly expect the flexibility to switch between virtual consultations and physical visits without disruption.
Telehealth platforms must support seamless transitions between care modalities through unified scheduling, centralized patient records, and consistent clinical documentation. Systems that maintain care continuity across both virtual and physical interactions will better support provider workflows and improve patient satisfaction, aligning with how healthcare is realistically delivered.
3. Expansion of IoT and wearable device integration
Remote Patient Monitoring (RPM) is evolving beyond traditional connected devices. Modern telehealth ecosystems now integrate continuous glucose monitors, wearable fitness trackers, smart blood pressure monitors, smart scales, and sleep tracking devices.
These technologies generate continuous patient health data between consultations, enabling proactive and preventive care. However, the real challenge lies in standardizing, filtering, and presenting this data in a clinically meaningful way. Telehealth platforms that invest in advanced data engineering, interoperability standards, and intelligent alert systems will provide greater value to healthcare providers and patients alike.
4. Blockchain for secure and patient-controlled health records
Although still emerging, blockchain technology has the potential to address long-standing healthcare challenges related to data fragmentation, interoperability, and record security. Blockchain-based architectures allow patients to maintain ownership of their health records while enabling secure data sharing across providers.
Early implementations are already being tested in areas such as clinical trial data management, provider credential verification, and secure health information exchange. Telehealth platforms designed with blockchain-compatible infrastructure will be better positioned to adopt decentralized healthcare data models as adoption increases.
5. AR and VR transforming virtual patient Interactions
Augmented Reality (AR) and Virtual Reality (VR) technologies are introducing new capabilities in telemedicine, particularly in areas requiring visual interaction and immersive patient engagement. These technologies are being explored for remote physical assessments, mental health therapy sessions, rehabilitation programs, surgical training, and chronic pain management.
As AR/VR hardware becomes more affordable and widely adopted, telehealth platforms that support immersive patient experiences will gain a competitive advantage, particularly in specialized care segments such as physiotherapy, behavioral therapy, and post-surgical rehabilitation.
Take the Next Step Toward Scalable Telehealth Success
Telehealth is rapidly becoming a core part of modern healthcare delivery, and organizations that act now will be better positioned to meet growing patient expectations and industry demands.
Building a successful telehealth website requires more than basic virtual consultation features—it demands secure architecture, seamless clinical workflows, regulatory compliance, and scalable technology that supports long-term growth.
Partnering with an experienced healthcare development team can significantly reduce implementation risks and accelerate time-to-market. With proven experience in building platforms like MedCall and TelaSight, Monocubed helps healthcare providers, startups, and enterprises develop reliable, HIPAA-compliant, and patient-centric telehealth solutions tailored to real clinical and business needs.
If you are planning to launch or upgrade your telehealth platform, now is the time to define your requirements, evaluate your development approach, and collaborate with experts who understand healthcare technology.
Taking a strategic, compliance-first approach today will help you deliver better patient experiences and build a future-ready virtual care ecosystem.
Build a Telehealth Platform Patients and Providers TrustWith
With proven healthcare development experience and compliance-first architecture, Monocubed delivers scalable telehealth solutions that support modern healthcare delivery and business growth.
Frequently Asked Questions About Telehealth Website Development
-
How much does telehealth website development cost?
Telehealth platform costs range from $40,000 to $500,000+ depending on scope and complexity. A basic MVP with video consultations, scheduling, and patient profiles typically costs $40,000-$80,000. A mid-range platform with EHR integration, ePrescription, and advanced messaging falls in the $80,000-$200,000 range. Enterprise platforms with multi-specialty workflows, remote patient monitoring, AI features, and comprehensive integrations can exceed $200,000-$500,000.
-
What are the compliance requirements for a telehealth platform?
In the United States, HIPAA compliance is mandatory for any platform handling protected health information. This includes implementing the Privacy Rule governing PHI use and disclosure, the Security Rule mandating technical, administrative, and physical safeguards, and executing Business Associate Agreements with every third-party service that touches patient data. Platforms serving international patients must also comply with GDPR, PIPEDA, or other regional data protection laws. Technical requirements include AES-256 encryption at rest, TLS 1.2+ encryption in transit, multi-factor authentication, and comprehensive audit logging.
-
How long does it take to build a telehealth website?
An MVP telehealth platform with core features takes approximately 3-4 months to develop with a dedicated team. A full-feature platform with EHR integration, ePrescription, remote patient monitoring, and advanced analytics requires 8-14 months. Key factors affecting timeline include stakeholder decision speed, EHR vendor certification processes, regulatory review requirements, and the development team’s healthcare domain experience. Teams experienced in HIPAA and healthcare data standards consistently deliver faster than those learning healthcare while building.
-
What is the difference between a telehealth website and a patient portal?
A telehealth website is a care delivery platform that enables real-time clinical interactions through video consultations, messaging, prescriptions, and appointment management. A patient portal is an information access platform that allows patients to view health records, lab results, billing history, and appointment schedules. While both are secure, web-based healthcare platforms, their core purposes are different. Many modern telehealth systems incorporate patient portal functionality, combining care delivery and information access in a single integrated experience.
-
Should I build a custom telehealth platform or use a SaaS solution?
The right approach depends on your organization’s needs. Custom development suits organizations with unique clinical workflows, deep integration requirements, competitive differentiation goals, or plans to offer telehealth as a core product. SaaS platforms like Doxy.me are appropriate for solo practitioners and small practices needing basic video consultation capability without development investment. White-label solutions offer a middle ground with faster launch but limited customization. Consider your five-year total cost of ownership, since cumulative SaaS licensing fees can exceed custom development costs for growing organizations.
-
What technology stack is best for telehealth development?
The most common and effective stack for telehealth combines React.js with Next.js on the frontend, Node.js with NestJS or Python with FastAPI on the backend, PostgreSQL as the primary database, and Twilio or Daily.co for HIPAA-eligible video communication. Cloud infrastructure should use AWS, Azure, or GCP with signed BAAs. EHR integration uses HL7 FHIR standards, and payment processing goes through PCI DSS-compliant providers like Stripe. The optimal stack depends on your specific requirements, existing infrastructure, and long-term scalability needs.
 By Yuvrajsinh Vaghela
By Yuvrajsinh Vaghela



